Detecting breast cancer early is pivotal to successful treatment. Our breast cancer program gives patients access to the most accurate and effective diagnostic tests available. Common diagnostic tests include:
Regular Breast Exams
A physical breast exam performed by a doctor checks for any lumps or irregularities. Women can also perform monthly self-exams at home.
Mammograms
X-ray imaging of the breast that can reveal tumors or irregularities. Recommended annually for women over 40.
3D Mammography
An advanced form of breast imaging that uses X-rays and computer reconstructions to create a three-dimensional picture of the breast.
Magnetic Resonance Imaging
(MRI)
Imaging that uses radio waves and magnets to create detailed images that can show abnormal breast tissue.
Removal of breast tissue samples that are examined under a microscope to check for cancer cells.
Analyzing genes such as BRCA1 and BRCA2 to see if a woman has a mutation that increases her cancer risk.
Have you tested positive for BRCA1?
See our guide to unraveling BRCA gene mutations and breast cancer risk.
Non-Cancerous Breast Disease
Some non-cancerous breast diseases may cause pain or discomfort, lumps, nipple discharge, and other symptoms while others go completely unnoticed until found during a mammogram. Additional testing like a biopsy may be necessary to confirm an abnormality is not cancer. Common types of benign (non-cancerous) breast diseases include:
Fibrocystic Breast Changes
Lumpiness and cysts that come and go with the menstrual cycle. Very common and not harmful.
Fibrodenomas
Benign solid tumors made up of breast lobules and stroma. Often found in younger women.
Intraductal Papillomas
Benign tumors that grow in the breast ducts and can cause nipple discharge.
Excessive growth of lobules that can appear worrisome on mammography.
Fat Necrosis
Hardened breast tissue caused by damaged fat cells. Can be painful.
Mastitis
Inflammation of the breast, often caused by breastfeeding.
Duct Ectasia
Widening of the milk ducts that causes nipple discharge. More common in older women.
Granular Cell Tumors
Uncommon benign growths found in the breast lobules.
Atypical lobular hyperplasia (ALH) and atypical ductal hyperplasia (ADH)
Abnormal cell growth that increases future breast cancer risk.
Types of Breast Cancer
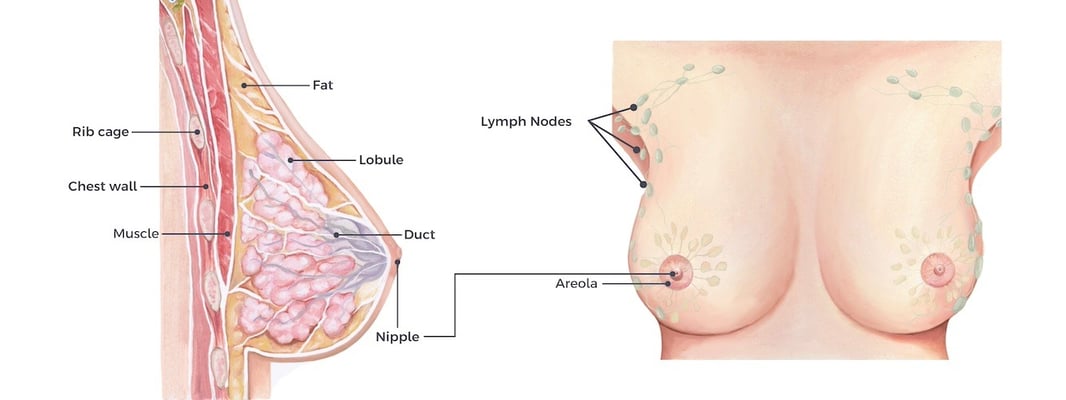
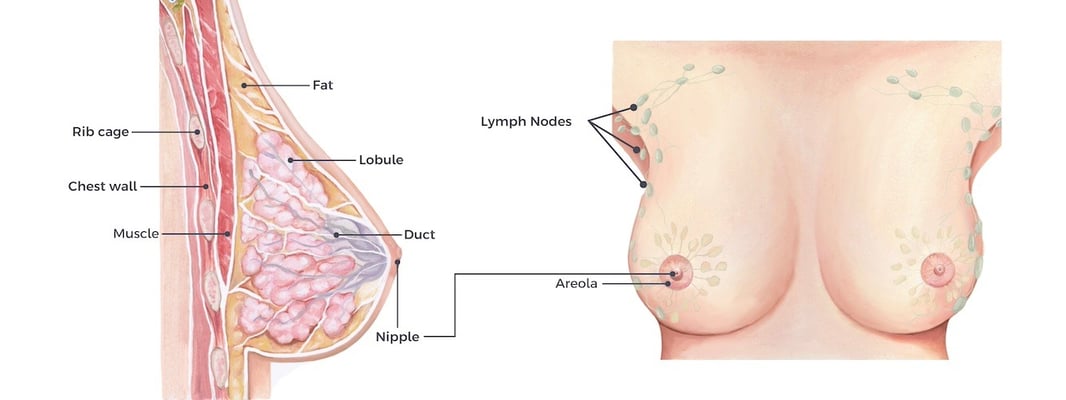
Breast cancer starts when cells in the breast grow out of control. Breast cancer is not just one disease, but rather includes several distinct types that arise from different parts of the breast tissue. The major categories of breast cancer include ductal carcinoma, which begins in the milk ducts, and lobular carcinoma, which starts in the milk-producing glands.
Carcinoma in Situ
Carcinoma in situ refers to early stage breast cancers that have not spread beyond their site of origin. The two main types are ductal carcinoma in situ (DCIS), which starts in a milk duct, and lobular carcinoma in situ (LCIS), starting in a milk-producing lobe. Though not life-threatening, carcinoma in situ may become invasive over time without treatment.
Invasive Breast Cancers
Invasive cancers have broken through normal breast tissue barriers and spread to surrounding tissue. Localized invasive cancers remain in the breast, while advanced invasive cancers spread beyond the breast. Invasive ductal carcinoma is the most common type. Stages 1-3 are considered early to locally advanced cancers.
Inflammatory Breast Cancers
Inflammatory breast cancer is a rare, aggressive form comprising 1-5% of breast cancers. It grows quickly and blocks lymph vessels in the skin, causing redness, warmth, and swelling of the breast, giving it an inflamed appearance. It is considered advanced cancer at diagnosis.
Recurrent Cancer
Recurrent cancer refers to breast cancer that comes back after initial treatment. It may reappear in the same site as the original tumor or in other parts of the body. Recurrence indicates the cancer was not completely destroyed with initial therapy.
Stages of Breast Cancer
The stage of breast cancer describes how far the cancer has spread from its original site at the time of diagnosis. Determining the stage is critical for selecting the best treatment approach. Breast cancer staging typically ranges from stage 0 to stage IV based on tumor size, lymph node involvement, and metastasis (the spread of cancer cells from the original tumor site to other parts of the body). The stages of breast cancer are:
- Stage 0: Also called carcinoma in situ. Abnormal cells are present but have not spread.
- Stage I: Tumor is 2 cm or less and has not spread to lymph nodes.
- Stage IIA: No tumor in the lymph nodes but cancer is 2-5 cm large.
- Stage IIB: Tumor is larger than 5 cm but has not spread to lymph nodes.
- Stage IIIA: Tumor is 5 cm or smaller and has spread to 1-3 axillary lymph nodes or nodes near the breastbone.
- Stage IIIB: Tumor has spread to tissues near the breast or more lymph node involvement.
- Stage IIIC: Cancer is extensive in the lymph nodes.
- Stage IV: Cancer has metastasized or spread to distant sites like the liver, lungs, bones, or brain.
Treating Breast Cancer
The main treatments for breast cancer include surgery, radiation therapy, chemotherapy, hormone therapy, and targeted drugs. Treatment is tailored to each patient based on the type and stage of cancer, as well as age, overall health, and personal preferences. Some breast cancers can be treated with radiation therapy alone. However, we often recommend even small, early-stage tumors be removed. Our surgeons are specially trained and experienced in performing the following breast cancer surgeries:
Breast Surgery
The goal of breast surgery is to remove the tumor (and in some cases, the affected lymph nodes). Breast surgery may be followed by radiation therapy to kill any remaining cancer cells. There are two primary types of breast surgery for cancer removal lumpectomy and mastectomy.
Lumpectomy
Also referred to as partial mastectomy or “breast conserving surgery,” a lumpectomy is performed when the tumor is relatively small and contained in one area of the breast. During the procedure, the surgeon removes the tumor and some normal tissue around it while preserving the breasts natural shape and appearance.
Mastectomy
A mastectomy is an extensive procedure that removes the entire breast and nipple. In severe or late-stage cancer, this surgery may also involve removing some or all axillary lymph nodes and chest wall tissue. Fortunately, women can opt for delayed or immediate breast reconstruction surgery to restore the appearance of a natural-looking breast.